Archive for year: 2020
Agile Decision Making: Combining Insights with Instinct to Navigate the Unknown
Decisions are being made today that may alter a healthcare organization’s trajectory for years to come. The pandemic has revealed how unprepared we are as an industry to use real-time and predictive data to tell us “what is happening”, “what will happen” and “how do we make it happen.”
COVID-19 has upended conventional leadership thinking and challenged even the most astute to admit “we don’t know what we don’t know.”
We Must Think Differently
In recent years, the healthcare industry has made a significant investment in advanced analytics and encouraged a transition to insight driven decision making. A survey of healthcare executives conducted by Black Book in January 2020, indicated that the vast majority (93%) feel data analytics is crucial to helping meet future healthcare demands and make strategic decisions. Yet, utilization of advanced analytics was described as “negligible” by 80% of the respondents. 71% of surveyed executives said they were too busy to learn such systems. In our conversations with healthcare leaders, they indicate they prefer to delegate analysis to others, aren’t really aware of what data analytics options they have, and often prefer to rely on their instinct – after all, it’s what made them successful.
For many, they have relied on the hundreds of static spreadsheets and score cards providing weekly, daily, monthly, and quarterly reports on “what happened” to validate these instinctual decisions. Yet, in today’s world much of this history is not pertinent. Comparative benchmarks, based on pre-COVID operating models, are no longer valid. Even the most sophisticated data scientists cannot take this historic data, identify new patterns and build a model to predict the future based on our current circumstances in a rapid fashion. Even the fastest computer processor can’t generate the algorithms we need when the situation changes as rapidly as it does today. Advanced analytics tools such as machine learning and predictive modeling are at their best when the future environment is similar to the historic environment – and that’s not the case today!
Healthcare decision makers must think differently about the role of data in their decisions and their approach to making decisions.
Agile Analytics, Combining Insights & Instinct for Decision Making
In the emerging COVID world, decision makers need practical, short term, results driven answers to their questions. Influenced by interrelated factors such as numbers of positive cases, bed availability, medication and PPE supply, treatment protocols, deployment of virtual tools and the impact of social determinants on population segments, the problems we are trying to solve change constantly.
Agile Analytics is a new paradigm for healthcare decision makers and is focused on rapidly finding value in data.
COVID brings the need for quick turnaround of information and rapid decisions. Historic data trends and traditional, large scale analytics projects are not dynamic enough nor nimble enough to support today’s decision-making environment. Since “we don’t know what we don’t know”, we must learn along the way. Jumping to solutions, based on traditional best practice or the play books of the past may lead us down the wrong path. Yet, complex architectures and advanced analytics platforms may not be responsive enough to meet the challenges of the current environment.
Agile Analytics is a style of working and problem solving. Originally created by software developers in 2001, agile is a collaborative approach built on short one to three-week iterations resulting in a data output that can be used to solve a problem or make a decision. Each targeted iteration starts simply, explores key components of the problem and initial hypothesis, and provides decision makers directional insights to drive data stories and resulting conversations.
The Minimum Viable Analysis
A Minimum Viable Analysis (MVA), is similar to the Minimum Viable Product concept developed by Eric Reis of Lean Start-Up fame. “Rather than spending months even years perfecting a product (analysis) without ever showing it to a customer (decision maker)…we start with a simple prototype of the product (analysis) get feedback from the customer (decision maker) and learn, then build it out further through multiple feedback sessions and iterations.”
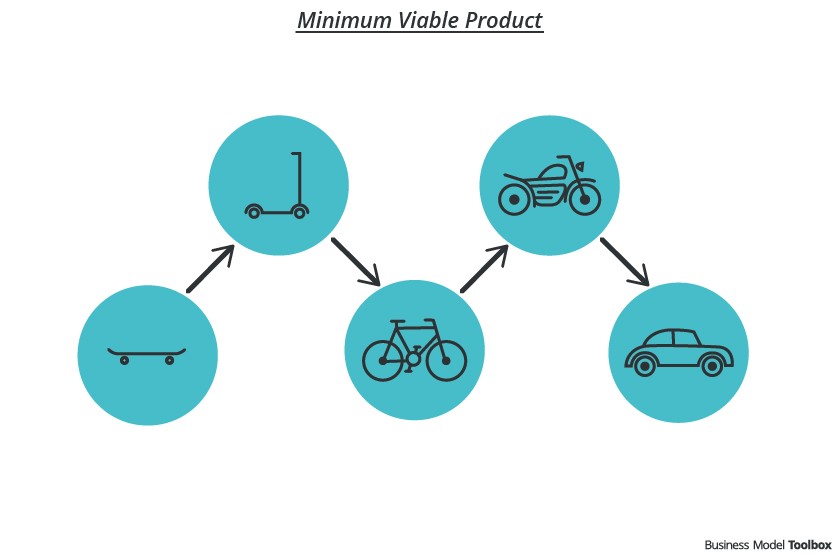
The MVA starts simply. As in the case of the minimum viable product, an initial problem to be solved or decision to make is identified by a small collaborative team of decision makers and data analysts. Using a travel analogy, rather than building an entire automobile to solve a transportation problem, the team starts with a skate-board as an initial prototype. This prototype defines data output, visualization or presentation expected from the MVA.
For problems the healthcare delivery organization is trying to solve during these times of uncertainty, a minimum viable analysis can be used to answer questions such as:
- When will we run out of ICU beds/ventilators?
- What staffing constraints will we have in acute care? in ambulatory? in post acute?
- What is changes should we make in our care model given the mix of virtual and in-person visits?
- What triggers will change our plans for rescheduling visits and procedures?
- Will we have PPE limitations or other supply chain issues?
Then, as specific questions are answered, an iterative approach can be used to add to the knowledge base and analysis to produce answers to more targeted questions or broader concerns.
We term the gap between the data output from our agile analytics effort and the change in behavior required to solve the original problem as the “Last Mile.” Unfortunately, the Last Mile is often an afterthought in analytics projects. Frequently, leading edge analytics initiatives don’t generate value or results due to ignoring the last mile. Resistance, lack of trust and transparency, siloed based behaviors, and a variety of last mile issues can often be anticipated and planned for early as problems and hypotheses are defined. Decision makers have a unique understanding of the environment where the desired insight-driven changes should occur. Instinct driven decision making plays an important role in defining Last Mile issues, early in the decision process.
COVID-19 brings a great deal of uncertainty, and decision makers can’t delegate data analysis as they did in the past. Multiple perspectives, judgement and experience are needed to collaboratively define the problems to be solved, potential hypotheses, explore the implications of analyses findings and communicate insight implications.
While data driven insights can provide new “aha’s”, they are best when combined with the decision maker’s instinct to navigate these uncharted waters.
Webinar Recording: Navigating Uncertainty: What’s in Your Analytics Playbook?
Navigating Uncertainty: What’s in Your Analytics Playbook?
Webinar recorded July 22nd, 2020. Hosted by Pam Arlotto and Susan Irby
Uncertainty brings opportunity for change. Throughout the COVID-19 crisis, healthcare leaders showed remarkable agility and worked collaboratively to deploy new virtual care models, innovate solutions to supply chain issues, and evaluate declines in revenue. As the healthcare industry continues to traverse through uncharted waters, analytics has become an essential navigational tool.
Conventional wisdom and the playbooks of the past may no longer be relevant. Decision makers must deal with uncertainty and think differently. Rather than relying on historic score cards to report “what happened”, leaders are using advanced analytics to explore “what-if” scenarios and model “what will happen” and “how do we make it happen”.
Decision makers should not defer this work to data scientists. They must play a central role in determining the problems to be solved, exploring what and how to analyze, and defining what the numbers mean to key decisions. Healthcare operations, financial, clinical, and business leaders must be able to engage, communicate and act using data driven insights.

During this webinar we examine:
- The Time Is Now for Advanced Analytics
- Five Game Changers for the Healthcare Decision Maker
- Continuing the Conversation: The Last Mile
Navigating Uncertainty: What’s in Your Analytics Playbook?
Lessons hospitals and health systems have learned from COVID 19
Over the past few months, hospitals and health systems have made tremendous transformations. They’ve had no choice. Rather than make decisions by committee and consensus, they’ve been forced to be agile, innovative and creative. Pam Arlotto, President and CEO of Maestro Strategies, is encouraging healthcare leaders to maintain that agility using data tools that enable prediction as they continue to navigate through uncertainty.
On July 28th, Pam Arlotto spoke with Don Seamons on episode 36 of the podcast, The Healthcare Solutions Project, on the topic of “Lessons hospitals and health systems have learned from COVID 19”


