Pam Arlotto was consulted by Healthcare Innovation on the scenario commonly referred to as “one foot in the boat, one on the shore” in the face of COVID-19.
Article by Mark Hagland on May 28th.
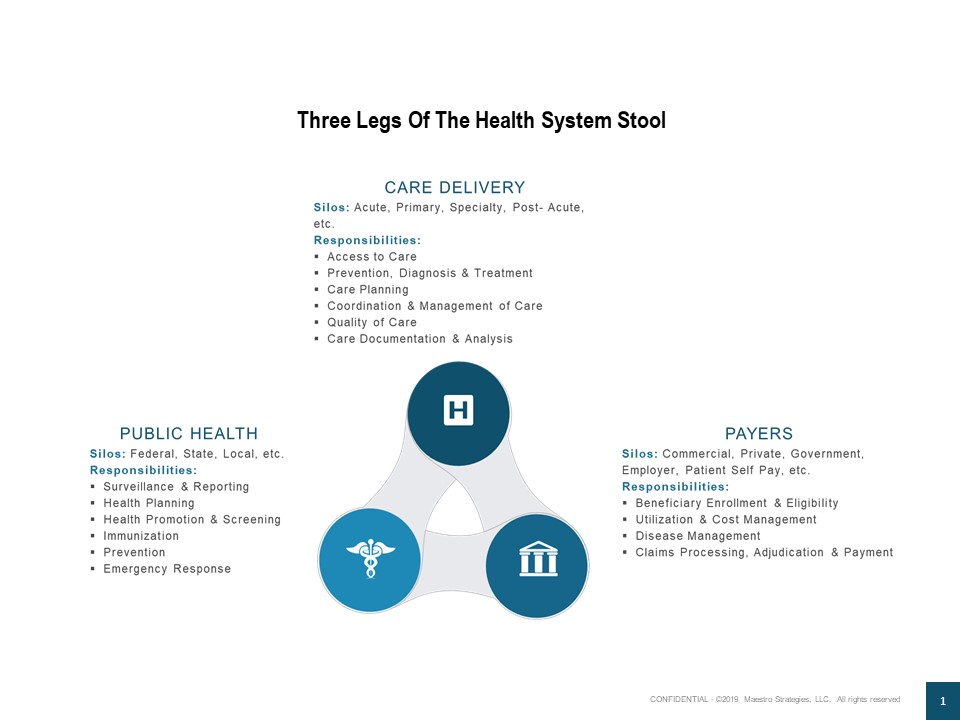
Pam Arlotto, CEO of the Atlanta-based Maestro Strategies consulting firm, notes that, “In our new book, Orchestrating Value: Population Health in the Digital Age, we suggest that part of the ‘two feet’ challenge is that value-based care and population health have been tacked onto the existing bricks and mortar delivery system. Our silo-based culture, hierarchical organization structures and conflicting incentives have created roadblocks and barriers to the transition.”
In that regard, Arlotto says, “Interestingly, times of crisis and chaos, force innovation and creativity. Rather than going back to business as usual, the healthcare industry has an opportunity to think differently as we go forward. COVID19 and its challenges drive collaboration across government, community, economic, care delivery and social sectors – ultimately, the very definition of population health. Arlotto notes that, “A recent survey by the National Association of ACOs (NAACOS) indicates that 94 percent of Medicare ACOs are “very or somewhat concerned” with COVID19’s impact on organizational performance. Many at-risk ACOS are weighing whether to quit the MSSP or Next Generation models. This could portend a very different business or operating model for the future.”
Indeed, Arlotto says, “Telehealth and digital health, for example, have already driven dramatic change in the ‘flatten the curve’ stage of the COVID19 crisis. As we move to the next stage, health systems will have to intentionally design hybrid (digital-plus-onsite) care delivery models in concert with regional plans that integrate public health, economic and social strategies to mitigate, manage and support patients and the broader population.”
Asked how she sees the issue playing out among hospital-based integrated systems in the next few years, Arlotto says, “We are working with a number of health systems to use advanced analytics strategies to inform their next stage hybrid strategies. Data provides insights on emerging patterns which can drive design of services, patient experiences and revenue implications. For most of our clients, this means combining traditional score cards with real time analytics and eventually moving into the predictive and prescriptive space – ultimately creating a new data ecosystem and platform.”