Untangling Complexity: Agile Decision-Making During the COVID19 Crisis
“The system is not really geared to what we need right now… let’s admit it,” said Dr Anthony Fauci from the National Institute of Allergy and Infectious Diseases.
The outcry for testing from patients and the media has challenged the US government, public health leaders and clinicians in primary care and hospital emergency rooms as they the battle the COVID19 pandemic. It is clear, the complexities of test development and deployment are only the tip of the iceberg as our fragmented healthcare system ramps up our response.
In an ideal world, the public health, care delivery, and payment systems are all components of a unified system – a three legged stool of sorts, guaranteed not to wobble and each carrying its respective weight in managing the health of the US population. Yet, in reality the three legs of the stool rarely collaborate. Each with their own ingrained cultural, political, regulatory and economic incentives. In this world, distinct responsibilities, bureaucratic processes and information systems burden decision making and slow down response.
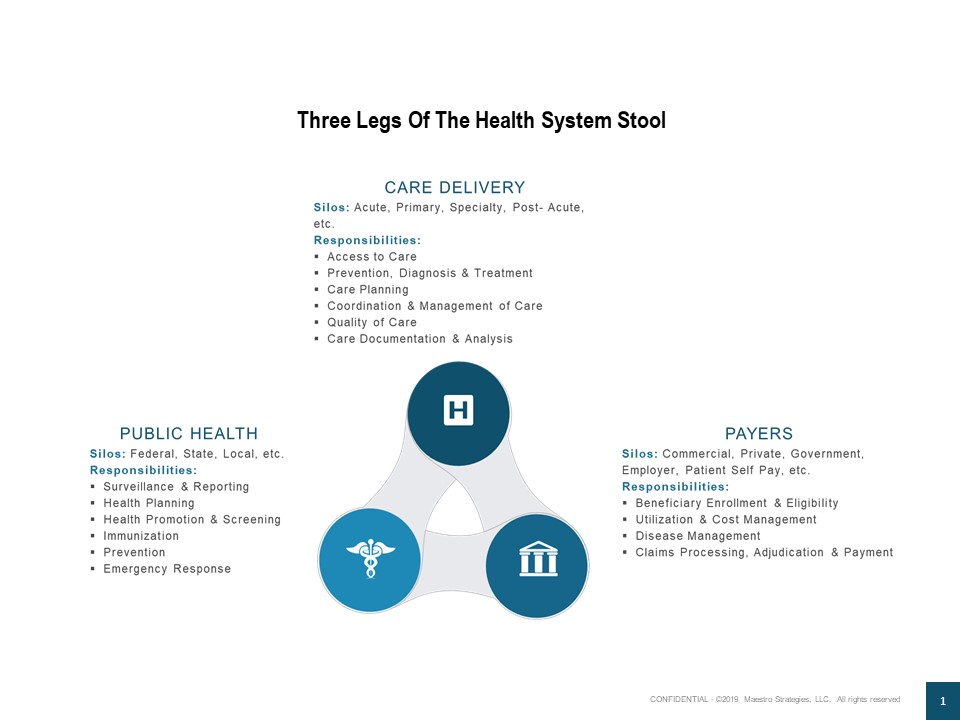
COVID19, knows no boundaries. In just a few short days, it is smashing the complicated mixture of federal, state, local, public and private organizational siloes and accomplishing more than many of us who have spent our careers trying to improve the system.
The March 17th expansion of telehealth benefits for Medicare recipients by CMS provides a tangible example. Relaxation of HIPAA rules gives the country’s older population access to medical care (both virus related and for other services) without having to leave their homes. Providers can use personal video chat applications like Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, or Skype. Rather than deploying technology for technology’s sake as we have done in the past, this step demonstrates:
- Coordination across the silos of public health, care delivery and payment
- Design of a new way of working – based on the needs of the at-risk population and their care providers
- An agile decision that simultaneously untangled the complexity of the current system
- Rapid communication of the change through multiple media channels
- Quick tools forwarded to patients and their clinicians from health care industry associations, data and technology partners and advisors
The 9-11 Commission reported, “The 9-11 attacks revealed four kinds of failures: in imagination, policy, capabilities, and management’ (National Commission on Terrorist Attacks upon the United States 2004, p.339). Today, as we face this threat each step we take provides an opportunity to untangle the complexity, remove barriers and set the course for more agile and unified decision making. What other steps should we take?