Research on Hospital Patient Portal Use
Dr. S. Luke Webster, a consultant with Maestro Strategies, was quoted in Modern Healthcare’s recent article, “Black, older patients less likely to use hospital patient portals.”
Read the full article here.
Dr. S. Luke Webster, a consultant with Maestro Strategies, was quoted in Modern Healthcare’s recent article, “Black, older patients less likely to use hospital patient portals.”
Read the full article here.
Many healthcare organizations see the use of analytics as a primary differentiator in the journey to value-based care. The current analytics vendor marketplace includes:
Most health systems use these systems for a variety of analyses including:
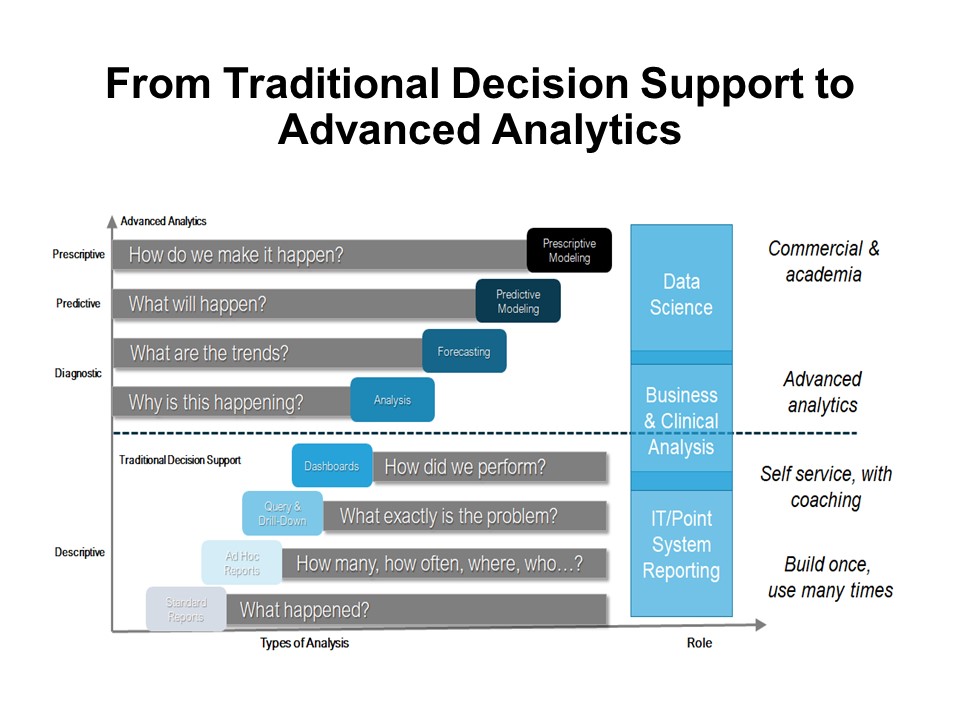 Advanced organizations are moving into Continuous Intelligence (CI). Rather than depending on traditional score cards, which require people to orchestrate every step in the analysis, CI uses artificial intelligence and machine-based algorithms to automatically interpret and harmonize the data. CI continuously discovers patterns and learns what’s of value in the data, and immediately sends insights to decision makers. In healthcare, this will be extremely valuable at the point of care, for care managers working across the continuum and for strategists who need agility in their decision-making processes.
Advanced organizations are moving into Continuous Intelligence (CI). Rather than depending on traditional score cards, which require people to orchestrate every step in the analysis, CI uses artificial intelligence and machine-based algorithms to automatically interpret and harmonize the data. CI continuously discovers patterns and learns what’s of value in the data, and immediately sends insights to decision makers. In healthcare, this will be extremely valuable at the point of care, for care managers working across the continuum and for strategists who need agility in their decision-making processes.
 Demonstration Projects Help “Test the Waters”
Demonstration Projects Help “Test the Waters”Yet, healthcare leaders often struggle with basic analytics projects. In fact, Gartner has uncovered an 85% failure rate on data projects. Ironically, this may be in part the result of executives trusting their gut rather than the insights derived from the data. Other problems include political, data quality challenges, limited data interpretation skillsets, resistance to change, governance, etc. It is often helpful, prior to jumping in the deep end of the analytics pool for the organization to first:
In other words, “test the waters” prior to diving in. A Demonstration Project provides the ability to learn about insight-driven decision making through the execution of a clearly defined project. The Demonstration Project works best with a limited scope, limited resource commitment and within a short time frame. An Analytics Demonstration Project focuses on data quality, building trust and deploying a consistent data management methodology. Insights can be channeled into performance improvement projects, strategic and operational plans or other pertinent initiatives.
Often a “See One”, “Do One”, “Lead One” approach works well — an outside analytics advisor partners with the organization and leads the first project, the advisor partners with the organization on the second project and in the third project, the organization leads the project with the advisor serving as a mentor. Preparation and starting the project well are essential elements for success and key steps include:
Organizations who leverage the strategic value of data to make informed decisions will be the ones who not only survive, but thrive.
One-week post #HIMSS19, blogs and articles are using phrases like “no one unifying theme”, “something for everyone”, “the invasion of non-healthcare high tech” and “the end of the EHR movement” to summarize the global conference key take-aways. Even though the exhibition showcased interoperability, artificial intelligence, telehealth, security, the internet of things, precision medicine and more, the focus was not on these technologies. In fact, a more subtle underlying reality was clear in both the education sessions and vendor booths. Data is the star of the show!
Data collection, data integrity and quality, data access, data for benchmarking and comparative analysis, data protection and safety, data as part of care management platforms, data analysis and prediction, data visualization and ultimately, the transformation of data into information each had the spotlight. Data and analytics vendors were certainly a major focus of the show. These vendors were not outdone by solutions which offered data a by-product of a much more comprehensive offering such as Enterprise Resource Planning or data embedded within cloud-based services designed to solve specific business and clinical problems such as readmissions. Moreover, CMS took center stage in multiple forums to discuss the Interoperability and Patient Access Proposed Rule. With a goal to touch all aspects of healthcare, from patients to providers to payers to researchers, “CMS hopes to break down existing barriers to important data exchange needed to empower patients by given them access to their health data,” CMS Administrator Seema Verma indicated. HIMSS even gotten directly into the act. Recognizing the importance of data and information, they have changed their vision statement from “better health through IT” to “better health through information and technology.”
Yet, even with all of this attention and applause its hard to reconcile the maturity of data initiatives in many health and healthcare organizations today and the challenges faced by many. For data to be valuable, data must be converted into information, information into insights, insights into decisions, and decisions into action. Unfortunately, many health and healthcare still manage their data assets within siloed organization structures. Turf battles are common. Data-related issues for decision makers often include:
According to thought leaders at SAP, “less than 1% of the world’s data in business is analyzed and turned into benefits”.
Creation of an organizational approach to standardizing management of data, or Enterprise Analytics Management System (EAMS), results in a defined, documented and deliberately managed set of priorities, polices, procedures and processes. The EAMS should address the collection, definition, analysis, interpretation, translation and presentation of data to a wide variety of audiences.
Objectives for the EAMS are to:
For data to truly be the star of the show, we must improve our ability to govern and manage this critically important asset.
by Pam Arlotto
Contributors: Susan Irby
Beyond Return on Investment: Expanding the Value of Healthcare Information Technology, 2nd Edition this updated and revised edition provides lessons learned from healthcare IT adoption and the opportunity to drive value realization. From providing a basic primer on ‘how-to’ complete a Return on Investment analysis for a single project to developing a comprehensive program of value management to support the transition to high value healthcare, this book addresses emerging trends, practical approaches and measurement methods to help drive value.
Beyond Return on Investment, 2nd Edition views IT as a strategic asset in the transformation of healthcare. Based on previous editions, this book updates and identifies the components of an integrated value management strategy including value driven decision-making culture, an integrated approach to strategy development, a value based governance model, a process that defines business case development through ROI analysis, value measurement and value scorecard development. New chapters in this addition include a Framework for Value Management, validating vendor defined value and ROI, and new methods for realizing value.
Available through CRC Press, order here.
Disruptive innovation in healthcare will depend on new combinations of data, technology and business models to create new interactions with health and healthcare consumers. In a NEJM Catalyst Marketplace Survey, healthcare executives, clinical leaders, and clinicians ranked the healthcare sectors in most need of disruption. The top three sectors were hospitals and health systems (65%), healthcare IT vendors (47%), and primary care (36%). Interestingly, a dichotomy emerged when respondents considered whether buyers were willing to pay for solutions to result in disruptive innovation. Most notably, health care IT shot to the top of the list, named by half of respondents. Hospitals and health systems were second (46%).
Yet according to a recent Health Data Management survey, 72% of respondents from healthcare organizations indicate that achieving EHR optimization is either extremely important or very important for their organizations. Healthcare leaders vary in their definition of optimization. For some it consists of routine maintenance, for others it involves remediation of technical issues not addressed during implementation, and for others it includes the addition of new functionality. The performance-improvement minded define optimization as including standardization of workflows, improved use of data and application of best practices. There are three problems with this thinking:
Disruptive innovation requires one to solve the business and clinical problems of the industry. These problems are big, complex and often beyond the control of individual practitioners and health systems. For the best lesson on addressing complex problems, we can look within our own industry. Cancer, once a death sentence, was the focus of doctors and researchers for years. The common thinking was that a single cure for all forms of the disease would be the answer. Physician Sid Mukherjee, author of book The Emperor of All Maladies, describes the first breakthrough. Sidney Farber, now known as the Father of Modern Chemotherapy, decided to focus exclusively on treating leukemia. By narrowing his focus Farber was able to make remarkable progress against this single condition. As a result, his work led to new protocols and treatments for other cancers. According to Mukherjee, “focusing microscopically on a single disease, one could extrapolate into the entire universe of diseases.” The healthcare industry can learn and apply this lesson – to solve solve large complex problems, first attack smaller micro-problems.
There exists a full spectrum of high-impact value that can be realized and created when investments in HIT and digital tools are applied to solving healthcare business and clinical problems. The Healthcare Value Pathway illustrates the next levels of value and return on investment.
Key steps include:
Oh, and what about technology? Technology is and will be pervasive in all that we do in health and healthcare. Consider as you design new innovations, potential high-impact or value-added technologies. Rather than “wagging the technology tail”, move beyond optimization to focus value through disruptive innovation.