Business Plans for Affiliated Provider Solutions & Services
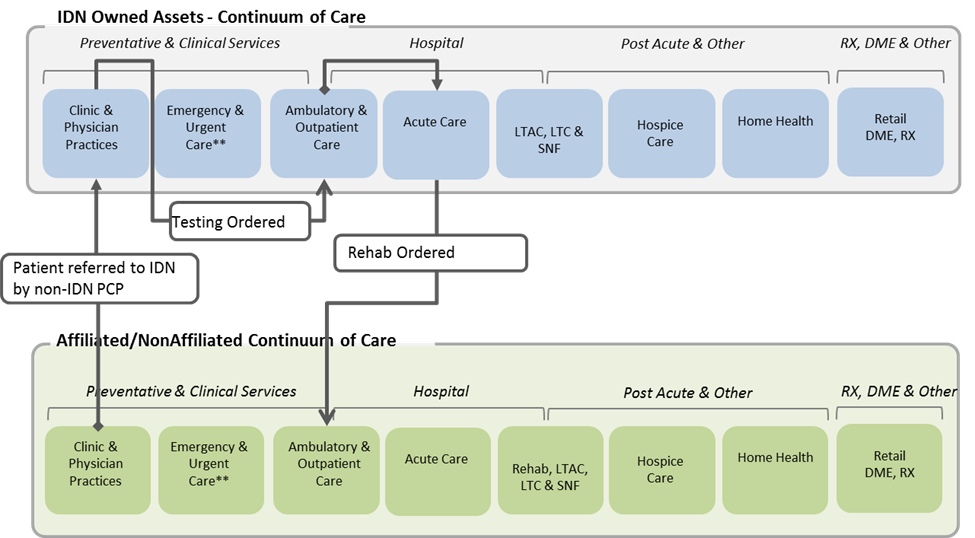
Despite the healthcare consolidation trend and the health system strategy to build a “System of Care” across the healthcare continuum, affiliated providers continue to be an essential element of the care delivery process in most communities. Even with strong referral management processes and systems, physicians will still refer patients to providers outside the “owned assets” of the IDN, patients will self-refer and primary care providers and specialists will create orders to be delivered outside the integrated delivery network. While most health systems are developing strategies to actively manage referral practices, even the most horizontally integrated health systems will be on a constant search for high-quality and low-cost affiliated providers to compete effectively in a value-based environment.
Affiliated provider programs at many health systems have struggled, even with the relaxation of the Stark Laws through the Safe Harbor provisions. Simply offering a donated EHR often fails to address the expanding scope of provider organizations (e.g., practices, skill nursing facilities, home health agencies, etc.) and often ignores the evolving demands of clinical integration and accountable care models which place greater emphasis on services and technologies that complement the EHR. Providers need effective application support services, enabling technologies such as telehealth, and a health system who is continually evaluating new innovations such as wearable technologies, mHealth, analytics, etc. that work with a myriad of EHR environments including donated EHR, web/portal/HIE, call centers, cloud based scheduling, fax and direct.
Developing a Business Plan that includes services and solutions for your affiliated providers doesn’t need to be overwhelming.
Suggested steps include:
- Step 1 – Recognize that your provider solution and service offering may start with physician practices, but will grow to include other provider settings. This may take time. While most markets share several similarities, there are unique factors that will determine when the business conditions of your market will support expanding the business plan and associated strategies to include additional care settings
- Step 2 – Develop a standardized services and solutions catalog that your customers need, is easily understood and can be delivered with a high degree of reliability. The services and solutions may be tiered or packaged to appeal to specific groups and level of integration, and specific variations may be designed-in to allow “localization” of based on unique requirements of specific entities, markets and specialties. Yet, the important point is that it is standardized, which by definition will produce a modest set of services and solutions. When a health system allows customizations, the services and solutions catalog expands and operating costs soar
- Step 3 – Resign yourself to the fact that your organization can’t do it all. Sourcing selected services and solutions from the catalog to value added resellers, Internet Service Providers, hardware providers, etc. will be important. The goal is to create a variable model that reduces risk, creates economies, and ultimately provides exceptional service
- Step 4 – Determine the business (i.e., operational, organizational, & financial) model that is right for your organization. There are a number of different models that can be used. What is right for your organization will depend on its operating strategy. Key questions include:
o Do you provide services through existing IT departments or management services organizations?
o How are the services provided to employed providers and owned entities?
o Is a separate services organization necessary to provide the services? Do you run the business as a profit center or cost center?
o Are multiple entities using the services and how do you share oversight and management? - Step 5 – Create the go-to-market plan. Communicating the value proposition and earning the trust of customers can be the most challenging component of any business plan. This is particularly true if previous attempt to align with affiliated providers have not been successful at your organization or neighboring health systems. Pre-emptively addressing concerns, demonstrating how services have been tailored to better meet needs, illustrating the executive support, and painting a long-term vision are all required for the program to thrive.
Maestro Strategies uses our collective experience gained assisting health systems with their provider programs as well as our work launching new companies, affiliations and agencies to help explore key strategies and associated operating implications to create a vision, build a business plan and design a road map for affiliated provider services and solutions. Please contact us a insights@maestrostrategies.com to discuss the unique needs of your provider community and how the steps above could be tailored to create a Business Plan for Affiliated Provider Services and Solutions to benefit your health system.