Disruptive Innovation v. EHR Optimization: Is the Tail Wagging the Dog?
Disruptive innovation in healthcare will depend on new combinations of data, technology and business models to create new interactions with health and healthcare consumers. In a NEJM Catalyst Marketplace Survey, healthcare executives, clinical leaders, and clinicians ranked the healthcare sectors in most need of disruption. The top three sectors were hospitals and health systems (65%), healthcare IT vendors (47%), and primary care (36%). Interestingly, a dichotomy emerged when respondents considered whether buyers were willing to pay for solutions to result in disruptive innovation. Most notably, health care IT shot to the top of the list, named by half of respondents. Hospitals and health systems were second (46%).
Importance of EHR Optimization
Yet according to a recent Health Data Management survey, 72% of respondents from healthcare organizations indicate that achieving EHR optimization is either extremely important or very important for their organizations. Healthcare leaders vary in their definition of optimization. For some it consists of routine maintenance, for others it involves remediation of technical issues not addressed during implementation, and for others it includes the addition of new functionality. The performance-improvement minded define optimization as including standardization of workflows, improved use of data and application of best practices. There are three problems with this thinking:
- At best optimization produces incremental performance improvement and change, resulting in a nominal return on investment and value,
- Second, optimization is focused on the technology not the healthcare business or clinical problem to be solved – resulting in the proverbial technology tail wagging the dog, and finally
- There is a perception that disruptive innovations must come from outside the industry, and if the data and technology leaders are “heads-down” focused on optimization, they may miss the chance to drive real change
Solving Narrow Business and Clinical Problems is the Key to Disruptive Innovation
Disruptive innovation requires one to solve the business and clinical problems of the industry. These problems are big, complex and often beyond the control of individual practitioners and health systems. For the best lesson on addressing complex problems, we can look within our own industry. Cancer, once a death sentence, was the focus of doctors and researchers for years. The common thinking was that a single cure for all forms of the disease would be the answer. Physician Sid Mukherjee, author of book The Emperor of All Maladies, describes the first breakthrough. Sidney Farber, now known as the Father of Modern Chemotherapy, decided to focus exclusively on treating leukemia. By narrowing his focus Farber was able to make remarkable progress against this single condition. As a result, his work led to new protocols and treatments for other cancers. According to Mukherjee, “focusing microscopically on a single disease, one could extrapolate into the entire universe of diseases.” The healthcare industry can learn and apply this lesson – to solve solve large complex problems, first attack smaller micro-problems.
Move to the Next Level of Value & Return on Investment
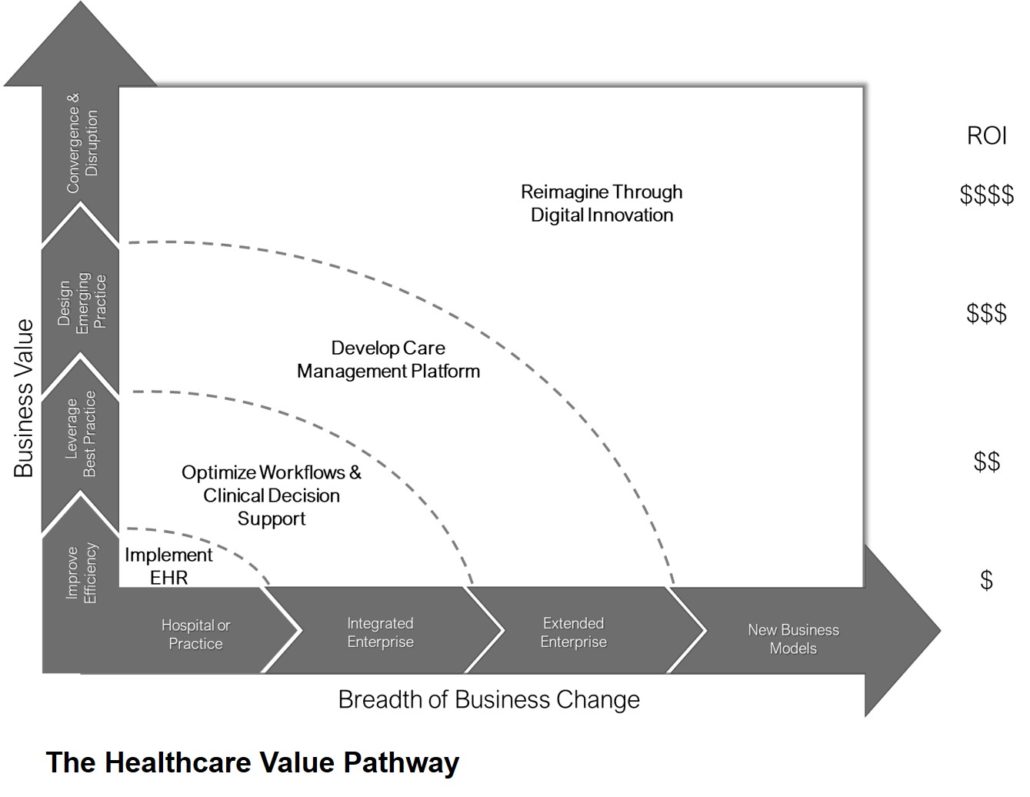
There exists a full spectrum of high-impact value that can be realized and created when investments in HIT and digital tools are applied to solving healthcare business and clinical problems. The Healthcare Value Pathway illustrates the next levels of value and return on investment.
Key steps include:
- First of all, start with a narrow focus on a specific problem such as the historic under-investment in primary care, the cost of a hospital stay, patients with multiple chronic conditions, the disparities in access or challenges in transitions of care
- Next explore specific innovations such as:
- Design new business and care delivery models
- Develop new networks new networks of patients and providers
- Create new approaches to sharing information
- Reinvent work processes, decision making structures and roles/responsibilities
- Analyze market, clinical, financial, claims, social determinant, etc. data to learn more about the problem to be solved
- Finally, iterate micro-phases of designing and piloting the innovation
Oh, and what about technology? Technology is and will be pervasive in all that we do in health and healthcare. Consider as you design new innovations, potential high-impact or value-added technologies. Rather than “wagging the technology tail”, move beyond optimization to focus value through disruptive innovation.